Until the day it dies, a cell that has become a skin cell remains a skin cell — or so scientists used to think. Over the past decade, it has become clear that cel- lular identity is not written in stone but can be rewritten by activating specific genetic pro- grams. Today, the field of regenerative medi- cine faces a question: should this rewriting take the conventional route, in which mature cells are first converted back into stem cells, or, where feasible, a more direct approach?
‘Terminally differentiated’ is a term that sums up the old way of thinking — that skin, muscle or other mature cells cannot be coaxed to adopt a drastically different fate. That idea began to falter a decade ago, when cell biolo- gist Shinya Yamanaka of Kyoto University in Japan showed that a handful of genes could transform adult fibroblast (connective tissue) cells into induced pluripotent stem (iPS) cells1. Like embryonic stem cells, iPS cells can develop into any cell type, a property called pluripotency. They can also be produced in unlimited quantities, unlike embryonic stem cells, which must be harvested from human embryos and therefore come with considerable political baggage.
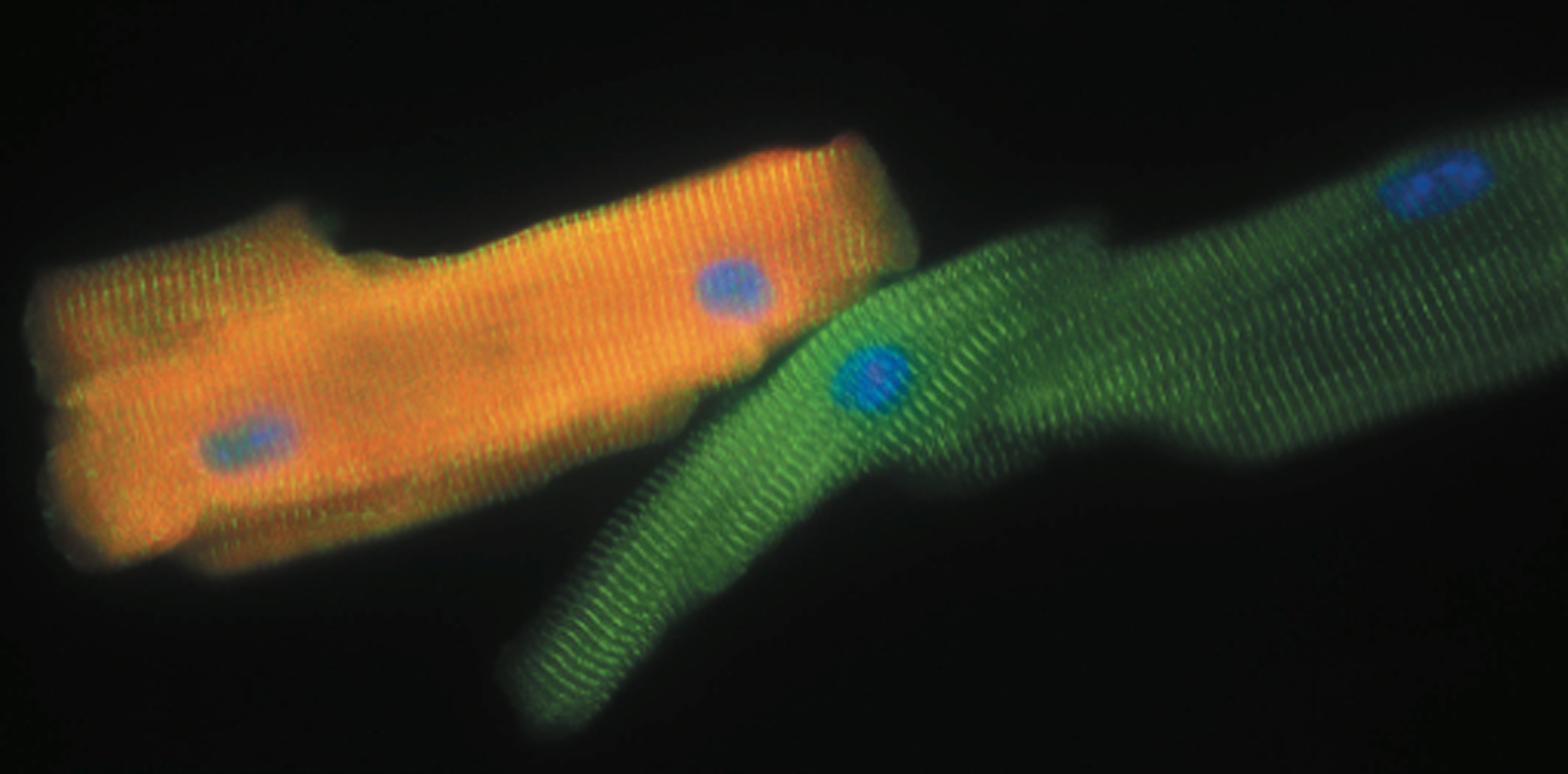
Just a few years after Yamanaka’s discovery — which earned him a share of the 2012 Nobel Prize in Physiology or Medicine — researchers began uncovering shortcuts for switching cell types that they called ‘direct reprogramming’. Mature cells of one kind could be coaxed to directly become another, with no pluripo- tent middleman. Researchers have learned how to turn skin cells into neurons or heart cells, and stomach cells into insulin-produc- ing pancreatic β-cells. “It’s amazing to watch the cells change right before your eyes,” says Benedikt Berninger of the Johannes Gutenberg University of Mainz in Germany, who uses direct reprogramming to generate neurons.
Research into direct reprogramming is more preliminary than work on iPS cells, but it is stirring excitement in regenerative medicine. Directly reprogrammed cells might be safer than cells that pass through a pluripotent state, because the latter share with tumour cells a capacity for extensive proliferation — making them potentially cancer-causing Trojan horses.
Clinical interventions based on iPS cells must be done carefully to ensure that no pluri- potent cells are transplanted along with the fully mature cells. “There’s a risk that you could lose control of these cells and that they start proliferating uncontrollably after transplanta- tion,” says Malin Parmar, a neurobiologist at Lund University in Sweden who hopes to use direct reprogramming to reverse the loss of neurons in people with Parkinson’s disease. “But if you bypass the pluripotent stage, it’s a lot quicker and potentially safer.”
CHANGING PROGRAMS
Rewriting cellular identities first requires an understanding of how those identities are established. Every cell in the body can trace its ancestry back to a single progenitor: the fertilized egg. As embryonic cells divide and mature, their destiny is determined by the spe- cific genes that are switched on and off over the course of development. Proteins called tran- scription factors regulate this process by bind- ing certain DNA sequences in the genome, and subsequently activating or suppressing adja- cent genes. The ones that govern the fate of a developing cell are often called master regu- lators because they operate at the summit of complicated cascades of gene activity.
“These master regulators are basically all defined by their pivotal roles in embryogenesis in the development of certain cell types,” says Qiao Zhou, a cell biologist at Harvard Stem Cell Institute in Cambridge, Massachusetts. “Perhaps a progenitor cell can become cell A or B or C, but if you force it to express a certain master regulator, it will inevitably choose A.”
An early demonstration of the usefulness of master regulators for direct reprogram- ming came as far back as 1987, when Harold Weintraub, Andrew Lassar and their colleagues at the Fred Hutchinson Cancer Research Center in Seattle, Washington, showed that forcing fibroblasts to express a certain por- tion of DNA put them on a developmental path to become muscle cells; they later discov- ered that the single gene responsible encodes the transcription factor MyoD2. “That was a paradigm-shifting observation, and people in the field thought that most other cell types would have that one key factor that would be powerful enough to convert the fate of a cell,” says Deepak Srivastava, a heart development researcher at the Gladstone Institute of Cardio- vascular Disease in San Francisco, California.
But it wasn’t that simple. The hunt for individual master regulators that could initiate reprogramming would yield many years of disappointment — until Yamanaka’s work on iPS cells revealed that the secret of effective repro- gramming was not a single factor, but rather combinations of multiple genes. As researchers started to mix and match different sets of mas- ter regulators, success stories began to emerge.
In 2008, Zhou was part of a team led by Harvard scientist Douglas Melton that trans- formed one type of pancreatic cell into another, generating the insulin-secreting β-cells that are needed by many people with diabetes. “Our study concluded that you need a minimum of three master regulators to make that happen,” says Zhou. In 2010, a group led by stem-cell scientist Marius Wernig of Stanford University in California turned fibroblasts into neurons, also using a trio of genes3. Further refinements and extensions of this work gave rise to a host of different, specialized neurons, with each type producing or responding to distinct neu- rotransmitter signals.
Most of these pioneering demonstrations of direct reprogramming have been achieved with cultured cells. Yet many researchers see much greater promise for regenerative medicine if cell conversions can be prompted inside the body. Pools of cells that are relatively abundant in an organ could be transformed into other kinds of mature cells that are more desperately needed. So far, there have been a handful of triumphs in animal experiments. Parmar’s group, for exam- ple, found that glial cells can be converted into functional neurons by injecting viruses laden with genes for reprogramming factors into the brains of mice. And Srivastava has likewise turned mouse fibroblasts inside the heart into beating cardiac muscle cells, a strategy that may offer a way to repair damage caused by a heart attack. “You’ve got this vast pool of cells that are already in the organ that you can harness for regeneration,” he says. But no one has so far tried direct reprogramming inside a human.
IDENTITY CRISIS
For now, most research is focused on ensur- ing the success of the reprogramming process. Investigators not only have to work out a suc- cessful combination of master regulators that turns on the genes that define a certain cell type: they also, ideally, have to discover the smallest possible set. This is because the most reliable way to force a cell to express master regulator genes is to deliver additional cop- ies of these genes to it, and delivering many genes into a cell is a much tougher technical challenge than providing just a few. Working out the minimal set of master regulators can be a slog: often the roster of candidate com- binations is huge, and the only way through a thicket of options is to systematically test each one. Parmar’s team started with 12 candidate genes for generating dopamine-producing neurons, for example, before eventually nar- rowing it down to 2.
Some researchers have started to create software specifically for direct reprogramming that incorporates information about which master regulators control the formation of tissues. A team spread over three continents has developed an experiment-planning tool called Mogrify4, which brings together large quantities of gene-expression data from a long list of cell types with rules about the gene net- works that different master regulators control. Mogrify uses these to predict the combination of reprogramming factors that will cause a desired cellular identity change. The idea is to provide researchers with a way to computationally identify the fewest possible master regulator genes that can directly reprogram one particular cell type into another.
But providing active master regulator genes isn’t always enough to ensure complete repro- gramming: the master regulators may successfully set a cell on a developmental path, but then leave it stranded in an immature, precursor state. Then the task is to identify which addi- tional genes must be active to finish the process, and add them to the delivery package.
Stem-cell biologist Hongkui Deng at Peking University in Beijing struggled with this problem for years. His initial efforts to directly turn skin cells into liver cells through the forced expression of master regulator genes alone yielded cells that failed to perform key, liver- like functions. Then, during a second round of screening, he identified additional genes that could complete the reprogramming5. He calls them maturation factors genes that are unimportant for initiating the conversion but crucial for obtaining functionally mature cells.
Other researchers have found that they can boost the success rate of direct reprogramming by augmenting the effects of master regulator genes with chemicals that act on cellular sig- nalling pathways to promote reprogramming — occasionally, chemicals alone can prompt a cell-type transformation (see ‘Better modifying through chemistry’).
Even with the appropriate gene and chemi- cal deliveries, it is hard to prove that any direct reprogramming is truly complete. Peering through a microscope can reveal whether a transformation has taken place — for example, whether flat, star-shaped fibroblasts have formed long, axon-like projections — but deeper analysis of the cell’s inner workings is also needed. Put simply, how can one be certain that a reprogrammed skin cell has truly become a neuron, and is not merely ‘neuron-like’?
Measuring the downstream activity of mas- ter regulator genes can offer insights into how well reprogramming has succeeded. If the introduced master regulators are doing their job, they should cause grand shifts in the overall patterns of gene expression in the cell nucleus, which should match the patterns found in mature cells of the target tissue. There are several ways to survey a cell’s total gene expression — for example, sequencing all of the RNA molecules in it. Researchers at Boston University and Harvard University in Massachusetts have drawn on this kind of data in their development of CellNet, a software program that can assess how well the gene activity in reprogrammed cells matches that of target cells6.
Still, the identity test that really matters is whether reprogrammed cells can functionally replace naturally differentiated cells. “If they look like neurons and have gene expression like neurons, that doesn’t mean they’re really neurons,” says Chun-Li Zhang, a neurobiologist at the University of Texas Southwestern Medical Center in Dallas. Convincing proof requires a battery of assessments, such as elec- trophysiological measurements that confirm whether a newly formed neuron is firing and is therefore capable of activating other neu- rons that are linked to it by synapses. No one characteristic can provide sufficient evidence in isolation, says Zhou. His group’s attempts to reprogram liver cells into pancreatic β-cells yielded only dysfunctional intermediates. “They synthesized and released insulin in large quantities — so much so that the animals died from hypoglycaemia,” he says. This is because the cells lacked pancreatic cells’ ability to sense and respond to blood glucose levels.
One of the findings of these diagnostic tests is that prompting reprogramming within a target organ often works better than efforts with cultured cells. “Most of our cells only partially reprogram to cardiac muscle when they’re on plastic,” says Srivastava. “But in their natural environment, the majority go all the way to a beating state, where they’re electrically coupled with their neighbours.” This may be due to chemical cues generated by other neighbouring cells in the organ, or because of features of the 3D tissue environment that are hard to replicate in the lab. Whatever the reason, it bodes well for developing clinical applications.
PATH TO THE CLINIC
Researchers agree that there are many hur- dles to overcome before these methods can be tested in people. In general, human cells have proven more challenging to directly reprogram than mouse cells: they tend to take longer to go through the reprogramming process and often require additional transcription factors to those that are sufficient in animal experiments.
Gene delivery also poses formidable challenges, especially into organs such as the brain. In some cases, viruses that preferentially infect particular cell types could help to guide repro- gramming factors to specific sites of disease or injury, but delivery to unintended sites may still pose risks.
Then there’s the issue of ‘robbing Peter to pay Paul’. Transforming glia into neurons in the brain reduces the number of glia there — which might pose a hazard. “These cells are not just for decoration,” says Berninger. “They have important functions, and how do we replace them if we take them away?” One possibility is to reprogram cells to a proliferative — but non-tumorigenic — neural progenitor state. That way, a few glia could yield numerous neurons.
Heart treatments are probably closest to the clinic. Srivastava’s team has already begun studies to turn fibroblasts inside pig hearts into cardiac muscle cells. “We have initial proof of concept that even in a big heart like ours, we can achieve efficacy,” he says. The team is now carrying out safety studies and refining their gene delivery method with the aim of gaining regulatory approval for human trials. Impor- tantly, heart fibroblasts are self-replenishing, so concerns over cell loss are less acute.
Zhou’s team is also making headway towards the clinic in its attempts to switch cultured human gastrointestinal cells directly into β-cells. The gut cells are easily obtained by biopsy, and after cultivation and reprogram- ming they could, in theory, be transplanted into the pancreases of volunteers who have diabetes.
Direct reprogramming is beginning to gar- ner interest from industry, although biotech- nology and pharmaceutical companies are not quite ready to jump in with both feet. Although research into iPS cells and embryonic stem cells has a head start in this respect, the gap may close as the advantages of direct cell-type switching come into focus. “There is not yet a comparable amount of resources and man- power going into this approach,” says Zhou. “But the field is quickly catching up, and I can’t wait to see where it’s going.”
Transcription factors are a natural choice for reprogramming overall gene activity, but the genes encoding them first have to be delivered into target cells. This process is laborious and raises potential safety concerns for clinical applications.
Chemical biologist Sheng Ding has found an alternative method: inducing direct reprogramming with cocktails of chemicals. In his lab at the Gladstone Institute of Cardiovascular Research in San Francisco, California, he has spent much of the past decade building a library of compounds that can greatly modify gene expression. Using chemical agents such as A83-01 and LDN193189, which can switch off certain cellular signalling pathways, Ding has successfully reprogrammed adult cells with no transcription factors whatsoever.
He thinks his approach is much less artificial because he externally triggers innate cellular mechanisms that lead to reprogramming, rather than abruptly forcing cells to produce proteins that they normally wouldn’t. “It’s really a gradual reprogramming process,” he says.
In a pair of recent experiments, Ding and his colleagues converted fibroblasts into neural stem cells7 and cardiac muscle8 by applying different cocktails, each consisting of nine different compounds, some of them pharmaceuticals. Although the results are impressive, heart researcher Deepak Srivastava, who collaborated with Ding at Gladstone on this work, notes that the heart muscle cells produced in this way are more developmentally immature than those reprogrammed with transcription factors.
But the approach offers far more precise control over reprogramming in cell culture than direct reprogramming with transcription factors alone, and advocates of Ding’s strategy think that it could avoid some of the regulatory complications around gene therapy. Only a handful of labs have tried this chemistry-alone approach, but many have quickly become converts, among them Hongkui Deng of Peking University in Beijing. “We see chemical reprogramming as the future,” he says. M.E.
_______________________________________________
Michael Eisenstein is a science writer based in Philadelphia, Pennsylvania.
1. Takahashi,K.&Yamanaka,S.Cell126,663–676 (2006).
2. Tapscott,S.J.etal.Science242,405–411(1988). 3. Vierbuchen, T. et al. Nature 463, 1035–1041 (2010).
4. Rackham,O.J.L.etal.NatureGenet.48,331–335 (2016).
5. Du, Y. et al. Cell Stem Cell 14, 394–403 (2014).
6. Cahan,P.etal.Cell158,903–915(2014).
7. Zhang,M.etal.CellStemCell18,653–667(2016). 8. Cao,N.etal.Sciencehttp://dx.doi.org/10.1126/science.aaf1502 (2016).

